What research has found its way into the email inbox recently?
Although singing is a nearly universal human behavior, many adults consider themselves poor singers and avoid singing based on self-assessment of pitch matching accuracy during singing (here referred to as singing accuracy), in contrast to the uninhibited singing exhibited by children. In this article, I report results that shed light on how singing accuracy changes across the lifespan, using data from a large online sample, including participants ranging from 6 to 99 years old. Results suggest that singing accuracy improves dramatically from childhood to young adulthood, unperturbed by voice changes during adolescence, and remain at a similarly high level for the remainder of life, exhibiting no strong tendency toward age-related decline. Vocal or instrumental musical training has significant positive effects on singing accuracy, particularly in childhood, though there was no evidence for gender differences. Finally, pitch discrimination varied with age similarly to singing accuracy, in support of views that singing accuracy reflects sensorimotor learning. Taken together, these results are consistent with the view that singing accuracy is a learned motor skill that benefits from engagement and can remain a fruitful endeavor into old age. (emphasis added).
citation: Singing accuracy across the lifespan
Peter Q. Pfordresher preprint article accessed 6-19-22 at https://nyaspubs.onlinelibrary.wiley.com/doi/10.1111/nyas.14815
Basically, this says that if you learned how sing accurately when you were young, you can probably sing well into your later years. And, since singing is a learned motor skill, one might assume that it can be learned even as one gets older.
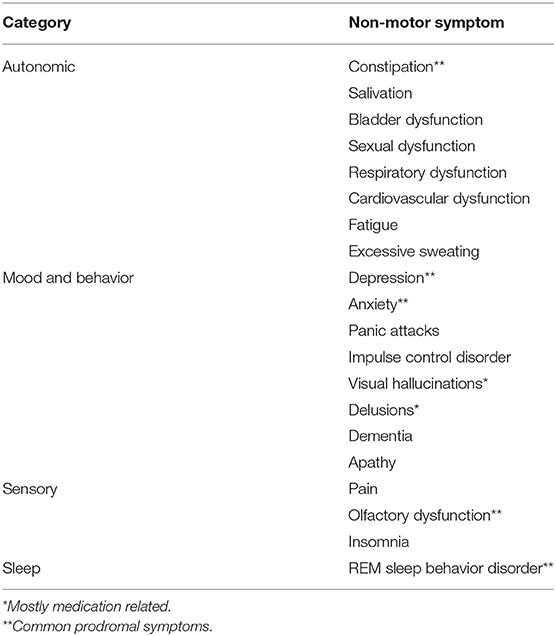
Relevance to folks with Parkinson’s Disease (PD)?
Vocal strength exercises, such as those provided by Power for Parkinson’s as free YouTube video classes, can help with specific Parkinson’s related symptoms:
Many people with PD speak quietly and in one tone; they don’t convey much emotion. Sometimes speech sounds breathy or hoarse. People with Parkinson’s might slur words, mumble or trail off at the end of a sentence. Most people talk slowly, but some speak rapidly, even stuttering or stammering.
Parkinson’s motor symptoms, such as decreased facial expression, slowness and stooped posture, may add to speech problems. These can send incorrect non-verbal cues or impact the ability to show emotion. Source: https://www.michaeljfox.org/news/speech-swallowing-problems accessed June 20, 2022 (emphasis added).
Since our vocal cords are muscles, and singing is a learned motor skill, we can strengthen those muscles and push against the progressive, degenerative symptoms of PD through exercises that:
- remind us to breathe deeply to sustain vocal volume,
- improve our posture in order to enable deep breathing,
- exercise the muscles of the face and mouth
- to enable crisp diction instead of slurring and mumbling, and that
- support emotional expression through inflection and singing.
And “Everybody Knows” that if exercise is fun, one is more likely to continue doing it.
Full disclosure: The author has attended Power for Parkinson’s ® vocal exercise classes since their inception in 2016, and co-founded a participant organized singing group (with the late Jeff Berke) in 2015. Therefore, he might be (definitely is) biased in favor of this modality of treatment for vocal and speech related symptoms of PD.
###