Just a look at the most recent shots:
Taken on December 1, 2021. Since March 27, I have seen and photographed at least one Monarch Butterfly in each of the following months in 2021. And that just doesn’t seem right…
Just a look at the most recent shots:
Taken on December 1, 2021. Since March 27, I have seen and photographed at least one Monarch Butterfly in each of the following months in 2021. And that just doesn’t seem right…
Diagnosis of PD is often not made until a person is in their 60s. With all the attention that has been focused on the disease(s) in the last 20 years or so, I suspect that more people are getting diagnosed at an earlier age, although most cases of young onset PD are likely to be genetic in origin.
However, an “early” diagnosis may not be a timely diagnosis, as the title of one opinion piece I read some time ago said (see link below).
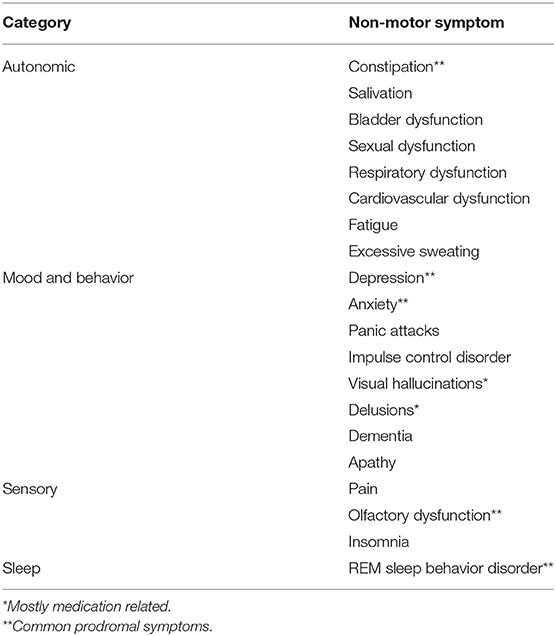
It is now becoming apparent that “Parkinson’s”includes several categories of symptoms, not just rigidity, tremors, and gait, as shown in the table below::
Source for the following table, accessed 11/28/2021: URL=https://www.frontiersin.org/article/10.3389/fneur.2020.00686
The problem is that treatment and diagnosis are often delayed until PD has already reduced Quality of Life for many folks.
Good evidence for the quality-of-life benefits of existing symptomatic treatment supports the argument for earlier diagnosis at a time when symptoms are already present (emphasis added). This argument would be significantly bolstered by the development of disease-modifying treatments. Benefits of early diagnosis and treatment would affect not only the individual (and their families) but also the wider society and the research community. Ultimately, however, shared decision-making and the principles of autonomy, beneficence, and non-maleficence will need to be applied on an individual basis when considering a “timely” diagnosis.
Therefore, the earlier one can predict the probability or inevitability of PD the sooner one can use treatments – whether pharmacological, surgical, nutritional, or lifestyle in nature – that can either reduce, delay, or defer (and possibly reverse?) the symptoms of PD.
Of all the symptoms associated with PD: tremors, bradykinesia, depression & anxiety, posture, gait issues (difficulties walking), REM Sleep Behavior Disorder (RBD), anosmia (loss of ability to smell), cognitive issues, facial masking, and micrographia (small handwriting) – RBD is the one which is most highly predictive of a later PD diagnosis.
The predictive ‘specificity’ is so strong that if someone has RBD, the chance of being diagnosed with Parkinson’s or related conditions over the next 15 years or more is over 80%
If an 18-21 year old person walked into a physician’s office with RBD, essential tremors, and depression as main symptoms, what would happen? In 1970, probably nothing – one might get treated for depression, but essential tremors are also called “benign”tremors, and were ignored, even if the patient reported being able to feel the tremors while resting, though invisible to the external observer. As for RBD, it would probably also be ignored.
By “a physician,” we are talking about a General Practitioner, or “family doctor,” and not s specialist like a Movement Disorders Specialist who would be trained to identify varied symptoms, including those that are prodromal. And, of course, the identification of prodromal symptoms has only been investigated within the last decade or so, and are identified as for “research only” purposes – not for clinical diagnosis. A recent survey article (not referenced below) indicated that a majority of general practitioners were either unaware of the Movement Disorders Society’s list of prodromal symptoms, or were not using them to make referrals to Movement Disorders Specialists.
But thanks to the dedication and generosity of folks like Michael J. Fox and others, PD has become a respectable disease for which the person who has it has no reason to be apologetic or ashamed, and can hold their head up (and they ought to, since one symptom is to walk with shoulders stooped down) and proudly proclaim that they have Parkinson’s, which is why they walk funny. And so it goes.
Articles that were quoted above or which contributed to this article are found in the links below.
But first:
An early diagnosis is not the same as a timely diagnosis of Parkinson’s disease
Prodromal REM Sleep Behavior Disorder and PD
10 Early Signs of Parkinson’s Disease / Parkinson’s Foundation
REM Sleep Behavior and Motor Findings in Parkinson’s Disease: A Cross-sectional Analysis
Current Update on Clinically Relevant Sleep Issues in Parkinson’s Disease: A Narrative Review
The prodromes of Parkinson’s disease
Exercise-Induced Neuroprotection of the Nigrostriatal Dopamine System in Parkinson’s Disease
###